As an independent NP, it may be a while before you have the means to hire support staff such as a manager or a billing specialist. Managing claims yourself is a steep learning curve that raises many questions about coding, including some concerning common CPT codes.
According to the American Medical Association (AMA), current procedural terminology (CPT) codes offer NPs “a uniform language for coding medical services and procedures to streamline reporting, increase accuracy and efficiency.” Such common standards and clinical descriptors promote uniform understanding for care delivered. In this introductory guide, you will learn a few best practices for CPT coding and examples of common CPT codes for nurse practitioners.
The Importance of Proper CPT Coding
CPT codes entered the healthcare world over 50 years ago. The CPT Editorial Panel is responsible for developing, managing, and updating CPT coding to align with changes and shifts in the healthcare landscape.
The AMA characterizes CPT terminology as, “the most widely accepted medical nomenclature used across the country to report medical, surgical, radiology, laboratory, anesthesiology, genomic sequencing, evaluation and management (E/M) services under public and private health insurance programs.”
On the practice side, proper CPT coding for nurse practitioners can help you avoid unpaid or rejected claims. It also can impart the value of NPs to payers as the coding reflects how they offer preventive care that closes gaps, especially for those with chronic conditions.
Tips for Common CPT Coding
Working in a traditional provider’s office, you have support staff checking to make sure everything is coded correctly. However, when you transition to practicing independently as an NP, there will be a learning curve when it comes to best practices in coding. Here are a few tips on how to avoid common CPT code mistakes.
- The expected combination of codes – Adding Category II codes (more on this later) has been made policy. For example, if you do an annual physical and codes concerning a patient’s chronic condition or tobacco use are missing, this could result in a claim being kicked back. Some EHRs can assist with this by not allowing a provider to close the chart when applicable codes are missing.
- Code to the highest specificity – The codes you use should be the most accurate match for what you are trying to code for. If a payer sees something that should have been a subclassification, they can reject the claim. In short, apply all applicable codes.
- As a rule of thumb, choose the code with the most digits. According to the American Speech-Language-Hearing Association’s website, “clinicians should assign 3-digit codes when there are no 4-digit codes within the category. Assign 4-digit codes if there is no fifth-digit subclassification for a particular category. Assign the fifth-digit subclassification code for those categories where it exits.”
- Code for your scope of practice/licensure – Caution is needed to avoid using codes that pertain to patient populations and specialties unrelated to your practice as an NP. Moreover, depending on the state you practice in, some NPs are not allowed to diagnose certain illnesses. While restricted NPs can code for follow-up care, issues can arise when using codes for initial diagnosis.
- Transition of care activities – When a patient is released from the hospital, you can miss out on reimbursement if no phone call is made – not that the claim would be incomplete, but rather that taking the step of calling the patient to come to a follow-up would increase the Medicare reimbursement.
- Document everything – The more your coding reflects a patient’s chart contents, the more accurate it will be. For example, social determinants of health (SDOH) are often omitted from coding. As mentioned earlier, you can get credit for calling the patient as part of their transition care management (TCM) visit after hospital discharge; however, detailed documentation of these efforts is imperative.
Categories for Common CPT Codes
Common CPT codes will fall under the following categories (as quoted from the AMA):
- “Category I – These codes have descriptors that correspond to a procedure or service. Codes range from 00100–99499 and are generally ordered into sub-categories based on procedure/service type and anatomy.
- Category II – These alphanumeric tracking codes are supplemental codes used for performance measurement. Using them is optional and not required for correct coding.
- Category III – These are temporary alphanumeric codes for new and developing technology, procedures and services. They were created for data collection, assessment and in some instances, payment of new services and procedures that currently don’t meet the criteria for a Category I code.”
A state Medicaid website shares more: “CPT Category II Codes are supplemental tracking codes used for performance measurement and data collection related to quality and performance measurement, including Healthcare Effectiveness Data and Information Set (HEDIS).” Category II codes are also frequently used along with ICD-10-CM codes.”
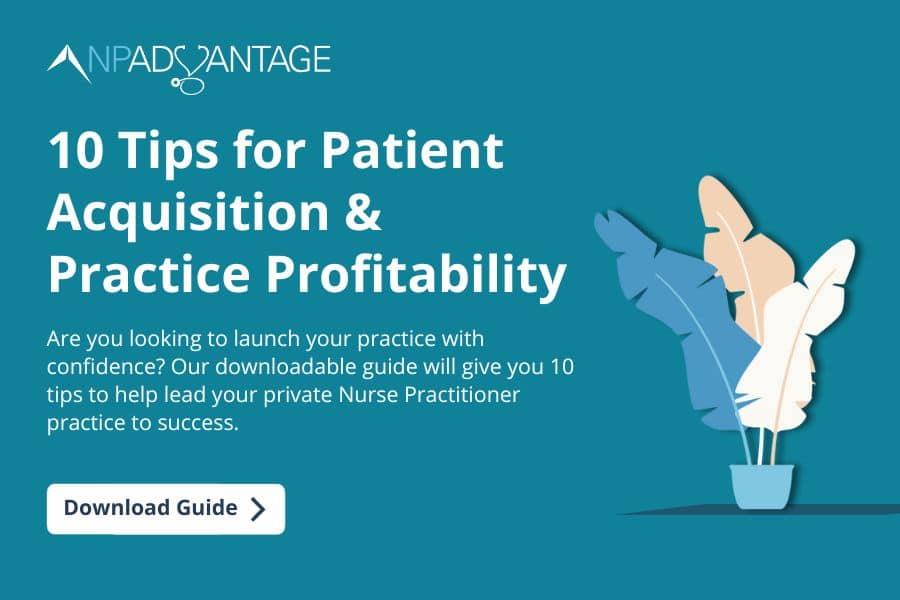
Common CPT Codes You Should Know as an NP
Common CPT codes involve:
- Routine annual visits
- Acute care
- Chronic condition follow-up care
- Evaluation and management
- Transition care management (TCM)
Get Help with Coding Through the NP Advantage Program
Getting your independent practice off the ground can feel like an uphill climb when you are trying to build a loyal patient base and keep the books balanced.
NP Advantage is here to help entrepreneurial NPs get their practices off the ground by offering an introductory no-fee support plan. Our blueprint for independent NPs includes coaching for nurse practitioner coding and outsourced billing.
Our support team:
- Improves current processes/workflows
- I
identifies areas of improvement - Strengthens NP’s knowledge about care management models/reimbursement opportunities
Reach out and get started on your success plan today.