As a nurse practitioner (NP), you’re always thinking about how to improve care for your patients. Maybe you’ve even been considering how to start your own private practice as a nurse practitioner yourself. A private practice gives NPs the flexibility of setting their work hours, choosing the services to offer, and tailoring care to the patient’s unique needs. Starting a startup nurse practitioner private practice can be a great way to take control of your career and provide the best possible care to your patients.
Starting and managing a successful nurse practitioner private practice is a comprehensive venture that requires careful planning along with patient-centered care. Marketing the practice and building a patient base, competition with other healthcare providers, dealing with insurance companies, and regulatory compliance are the main challenges that a NP faces when starting a private practice. Overcoming these obstacles requires creativity, resilience, and commitment, but for many NPs, owning their own practice is well worth the effort.
Navigating the Legal Requirements
Determining Your Scope of Practice
Obtain Licensure to Practice in Your State
Managing Your Credentialing and Enrollment Process
Creating A Business Plan
Considering NP Practice Operations
Growing Your NP Practice with Marketing
Managing Financials: Ensure Proper Reporting
Setting Up Your Practice’s New Internal Systems
Selecting An Electronic Health Records System For Your NP Practice
Payer Contracting and Revenue Cycle Management
Implementing a Telehealth System
The First Step: Navigating the Legal Requirements for Starting Your Own Nursing Practice
The first crucial step in starting a nurse practitioner private practice is ensuring legal compliance. Obtaining the necessary licenses and certifications is key in order to legally offer services as an independent healthcare provider. Familiarizing yourself with state laws and regulations governing private practices is also crucial to avoiding legal complications. Malpractice insurance is also a critical consideration to protect NPs in case of a malpractice suit.
Determining Your Nurse Practitioner Scope of Practice by State
Each state differs on the nurse practitioner scope of practice requirements you will need to provide. Naturally, you will need to know the scope of practice allowed in your state, whether that entails full practice authority, reduced practice, or restricted practice as you plan how to start a nurse practitioner private practice.
The American Association of Nurse Practitioners (AANP) has created an interactive national map showing which states govern nurse practitioner practices by which scope of practice. Regulations often vary within each nurse practitioner’s scope of practice, which is set by state legislatures, then often governed by the state’s board of nursing or board of medicine. You will need to ensure you’re up to date on the particulars for your state, but generally, scopes of practice involve the following guidelines:

Full practice states with full practice authority for nurse practitioners allow all nurse practitioners to evaluate patients; diagnose, order, and interpret diagnostic tests, and begin and manage treatments, including prescribing medications and controlled substances, according to the American Association of Nurse Practitioners.
Reduced practice states limit at least one element of the scope of practice, either limiting the settings of one or more elements of care or mandating a career-long regulated collaboration with another provider.
Restricted practice states limit at least one element of the scope of practice, requiring career-long supervision or management by another provider.
Obtain Licensure to Practice in Your State
Licensure requirements vary from state to state, so you need to know what your state requires. Check your state’s board of nursing website to review its requirements for becoming an independent NP. Some states require certain hours of supervised practice under a licensed physician, while others do not. Knowing what your state requires ensures that you can correctly follow the process and avoid mistakes.
Managing Your Credentialing and Enrollment Process
As a nurse practitioner, getting credentialed and enrolled with insurance companies is a critical step to achieving success in running your own independent practice. The following steps can help guide you through the process.
1: Gather necessary information: Before you start the credentialing process, gather all the required information, including:
- National Provider Identifier (NPI) number: 10-digit number that is used to identify healthcare partners, including all payers
- Malpractice insurance: Professional liability insurance that protects NPs from legal claims
- DEA registration: Unique identifier for a practitioner who can prescribe controlled drugs
- State license and hospital affiliations: Based on state scope of practice (SOP) acts, state medical and nursing board regulations, professional licensing, and other laws
Make sure all your documents are current and up to date before submitting any applications.
2: Research insurance companies: Research various insurance companies and identify which ones you would like to partner with. Evaluate their criteria for credentialing and enrollment, check if they offer reimbursement rates that align with your practice’s financing goals and determine whether they have a dominant patient population in your area of expertise.
3: Complete applications: Once you have chosen your preferred insurance providers, complete the credentialing and enrollment applications, ensuring they are error-free and complete. Sign and date all forms. Be aware of deadlines for submission and any additional information required before you can start billing patients.
4: Follow up on the process: Follow up regularly with the insurance providers to check the status of your application. Don’t be afraid to ask for the estimated timeline and next steps in the process, especially if you are applying for medicare, and be sure to keep track of all your communications and document everything.
5: Monitor and maintain credentials: After you’ve received your credentials and enrolled with your preferred insurance providers, maintaining your credentials is vital. Stay current with any requirements, such as continuing medical education credits, and renew them on time.
The Second Step: Creating A Nurse Practitioner Private Practice Business Plan
Setting up a private nursing practice can be a rewarding experience, but it requires an excellent business plan for success. Your independent NP business plan will help you articulate your goals and should:
1. Define your services: The first step to creating a business plan for your nurse practitioner private practice is to define the services you want to offer. You could offer primary care services, pediatric, or geriatric health services to name just a few. Define the services you want to offer clearly and ensure that the services are in demand in your area.
2. Identify your target market: The next step is to identify your target market. This involves researching the demographics of the community you want to serve. You could have a specific target market that you want to serve, or you could have a broad target market. For example, you could decide to serve children, adults, or the elderly based on the needs in your community.
3. Create a financial plan: The financial plan is the most crucial part of your business plan. It is essential to have a clear understanding of how much money will be needed to start and sustain your business. Often, NPs underestimate the amount of money they will need to start their private practice. By considering startup costs like marketing, rent, utilities, office equipment and supplies, staff salaries, and taxes, you’ll be able to set a sustainable budget. You also can hire a healthcare NP business consultant to help you prepare your budget and financial projections.
4. Set your prices: Setting your prices is a crucial aspect of your private practice business plan. The price you set for your services will determine your revenue. While service prices need to be competitive, rates should allow you to have a sustainable and profitable business. By researching what other nurse practitioners are charging in your area, you’ll be able to determine a pricing point that is competitive.
5. Define your marketing strategy: Once you have a financial plan and set your prices, you can identify tactics for attracting patients to your business. There are several ways to market your private practice, from social media and networking events to community outreach programs. After you’ve identified the marketing channels that your target market is most likely to use, you can develop a content marketing strategy that will generate leads and sales for your business. For busy NPs just starting out, outsourcing to consultants who specialize in healthcare marketing can help save them time and jumpstart their business.
Considering NP Practice Operations
You’re already familiar with how practices operate, and likely have experience with office workflows (billing, patient intake, etc.), and the use of technology like an EHR or telehealth. As you set up your practice, you’ll choose what to handle personally, what to delegate, and to whom.
Some office workflows are designed, while others are innovated. Opening your practice allows you to put the workflows you’re most confident in into place. You’ll also be able to adjust your business plan and workflows as patterns emerge and new efficiencies come to light. While time-consuming, the attention to detail here will decide how efficiently your practice operates, and ultimately, how well you serve your patients.
Growing Your NP Practice with Marketing
All businesses need to grow. Figuring out how to start a nurse practitioner private practice is no different. For that, you’ll need a marketing strategy. Your nurse practitioner independent practice marketing strategy should include a detailed plan for handling an optimized website, social media, SEO (Search Engine Optimization), digital advertising, and online reputation management.
Your nurse practitioner practice website will need to incorporate all these marketing elements to be an effective tool for promoting your new medical practice, drawing new patients, and keeping your current patients engaged with your practice for better patient outcomes.
Once it is properly tuned to work with a well-designed website, your marketing strategy will draw new patients seeking out quality care from reputable, capable, and caring nurse practitioners. That interest can be generated from an online search, paid ads, and the glowing reviews of satisfied, healthy, and happy patients.

Search Engine Optimization (SEO): When potential patients search for your services, they’ll likely look for services that your practice provides on Google and other search engines. Savvy SEO strategies can put you at the top of search results returned. This is an effective, organic method of marketing, where search engines detect your website is a high-quality source that will best serve the people looking for a nurse practitioner practice like yours.
Digital Advertising: On the other side of the coin, you can purchase Google ads for your nurse practitioner practice to make sure your business shows up throughout a potential customer’s daily browsing, opting for a paid approach to putting your practice in front of potential patients that Google’s algorithms determine may be interested in finding a nurse practitioner.
Online Reputation Management: Lists of local providers provide a prime opportunity to impress potential patients searching for a new nurse practitioner. Capitalizing on such lists includes encouraging ratings and reviews, and making sure you receive online praise when patients receive the great care you’re providing. Reputation management is a crucial part of marketing your practice. Online word of mouth is a very powerful marketing tool.
Take a look at Medical Advantage’s ebook on marketing your medical practice, which provides a handy guide on marketing your new nurse practitioner private practice for more guidance on bringing new patients into your practice.
For more guidance on bringing new patients into your practice, check out Medical Advantage’s E-Book on marketing your medical practice, which provides a thoughtful and easy-to-follow guide on marketing and growing your new nurse practitioner private practice.
Managing Financials: Ensure Proper Reporting
The bottom line of your business will need to be managed, not only to remain profitable but to ensure you can provide the level of care you set out to deliver with your nurse practitioner private practice. The most accurate, fastest way to collect financial data about your practice and present it in a useful report is through healthcare financial dashboards.
Healthcare financial dashboards track charges, claims by location, physician, insurer, and when they’re approved or denied, condensing that and additional information from multiple sources to inform financial business decision making.
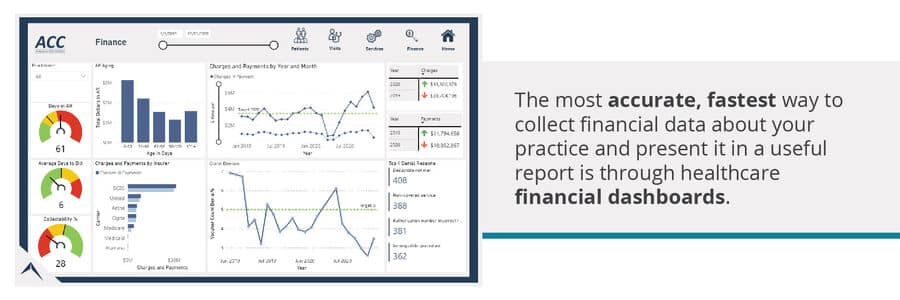
Population health dashboards and quality of care dashboards will also guide your practice.
A population health dashboard can collect and present information about your patients’ geography, age, and other demographic differences to illuminate health trends and guide treatment.
Quality of Care dashboards helps track quality metrics needed for reimbursement programs such as MIPS (Merit-based Incentive Payment System).
Setting Up Your Practice’s New Internal Systems
Medical practices require internal systems including contracting, electronic health records (EHR) software, payer contracting and billing, and telehealth software to operate smoothly and remain up to date.
Selecting An Electronic Health Records System For Your NP Practice
A modern practice will need to choose the right EHR software to manage records and essential business functions. What size is your practice? What do you want to share in your patient portal? Will your website interface securely with medical labs? Consider the full range of EHR needs before you decide. You will also want to ensure your software is set up for effective telehealth visits.
Setting up electronic health records software to manage patient records can be a daunting task. You will need to make sure your current staff is up to speed on the system, that new employees are trained to use it, and that it is user-friendly.
You may consider bringing in EHR consultants to help you set up the software for your practice. The effort will pay off by saving you time, and money and preventing frustration in the long run.
Payer Contracting and Revenue Cycle Management
Getting billing and contracting set up for business is a key first step before any medical practice can claim reimbursements and start bringing in revenue.
Your first step will be ensuring your providers are properly credentialed. Without credentials, your providers won’t be able to submit claims for payment for services provided.
The right revenue cycle management (RCM) software tools and training can help you better meet deadlines to maximize reimbursement submissions to payers.
With these systems in place, you will also need to set up training on the systems for staff members and make sure there’s a process in place to train new employees.
Implementing a Telehealth System
As telehealth gains traction, offering this service can bolster your patient reach and reduce costly no-shows by providing easier access to care. It often saves patients the hassle of attending physical appointments, as calls or video conferences are generally more convenient.
If you’re exploring telehealth, integrating it from the onset can distinguish you from other providers, enhancing the scope of care for your community.
It’s crucial to consider your telehealth solution when choosing your Electronic Health Record (EHR) system, as these two elements should seamlessly integrate, particularly during note-taking.
Setting up telehealth involves considering mobile video app portals for patient communication, the vendor’s IT support level, and EHR system integration to avoid unnecessary workload and prevent provider burnout.
NP Advantage Can Help
NP Advantage provides no-fee, no-hidden-cost solutions including everything you need to set up a nurse practitioner private practice. Partner with us and receive exceptional support from our experienced team of healthcare consultants and data analysts. We’ll set you on the best path for a bright future for your patients, and your practice.